Ritonavir Side Effects
Medically reviewed by Drugs.com. Last updated on Jan 11, 2024.
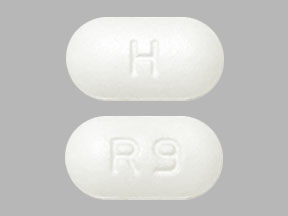
Applies to ritonavir: oral capsule liquid filled, oral powder, oral tablet.
Warning
Oral route (Capsule, Liquid Filled; Solution; Tablet)
Coadministration of ritonavir with several classes of drugs including sedative hypnotics, antiarrhythmics, or ergot alkaloid preparations may result in potentially serious or life-threatening adverse events due to possible effects of ritonavir on the hepatic metabolism of certain drugs. Review medications taken by patients prior to prescribing ritonavir or when prescribing other medications to patients already taking ritonavir.
Serious side effects of Ritonavir
Along with its needed effects, ritonavir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ritonavir:
Less common
- Fainting
- feeling faint, dizzy, or lightheaded
- feeling of warmth or heat
- flushing or redness of the skin, especially on the face and neck
- headache
- sweating
Rare
- Confusion
- dehydration
- dry or itchy skin
- fruity mouth odor
- increased hunger
- increased thirst
- increased urination
- nausea
- vomiting
- weight loss
Incidence not known
- Bloating
- chills
- constipation
- convulsions
- cough
- darkened urine
- decreased urination
- difficulty with breathing
- dry mouth
- fast heartbeat
- fever
- hives or welts, itching, skin rash
- increase in heart rate
- indigestion
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- loss of appetite
- loss of bladder control
- muscle spasm or jerking of all extremities
- noisy breathing
- pains in the stomach, side, or abdomen, possibly radiating to the back
- rapid breathing
- redness of the skin
- sudden loss of consciousness
- sunken eyes
- thirst
- tightness in the chest
- unusual tiredness or weakness
- wrinkled skin
- yellow eyes or skin
Other side effects of Ritonavir
Some side effects of ritonavir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Belching
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- change in sense of taste
- diarrhea
- dizziness
- general feeling of discomfort or illness
- heartburn
- lack or loss of strength
- sleepiness or unusual drowsiness
- trouble sleeping
- weakness
Less common
- Body aches or pain
- congestion
- delusions
- dementia
- difficulty with moving
- discouragement
- dryness or soreness of the throat
- excess air or gas in the stomach or intestines
- fear
- feeling sad or empty
- full feeling
- hoarseness
- increased urge to urinate during the night
- irritability
- lack of appetite
- loss of interest or pleasure
- mood or mental changes
- muscle pain or stiffness
- nervousness
- pain in the joints or in an unspecified location
- passing gas
- runny nose
- tender, swollen glands in the neck
- throat irritation
- tiredness
- trouble concentrating
- trouble swallowing
- voice changes
- waking to urinate at night
Incidence not known
- Gaining weight around your neck, upper back, breast, face, or waist
For Healthcare Professionals
Applies to ritonavir: oral capsule, oral powder for reconstitution, oral solution, oral tablet.
General
The most frequently reported side effects associated with this drug alone and in combination with other antiretrovirals were gastrointestinal (including nausea, diarrhea, vomiting, upper and lower abdominal pain), neurological disturbances (including paresthesia, oral paresthesia), rash, and fatigue/asthenia.
When used as a pharmacokinetic enhancer, side effects were dependent on the coadministered protease inhibitor. The manufacturer product information for the coadministered protease inhibitor should be consulted.[Ref]
Gastrointestinal
Very common (10% or more): Diarrhea (including severe with electrolyte imbalance; up to 67.9%), nausea (up to 57.4%), vomiting (up to 31.9%), upper and lower abdominal pain (up to 26.4%), dyspepsia (up to 11.5%)
Common (1% to 10%): Flatulence, gastrointestinal (GI) hemorrhage, gastroesophageal reflux disease, mouth ulcer, pancreatitis, increased amylase, constipation, circumoral paresthesia, local throat irritation
Frequency not reported: Abnormal stools, bloody diarrhea, cheilitis, colitis, dry mouth, dysphagia, eructation, esophagitis, esophageal ulcer, fecal incontinence, gastritis, gastroenteritis, GI disorder, GI symptoms, gingivitis, ileitis, ileus, melena, oral moniliasis, periodontal abscess, pseudomembranous colitis, rectal disorder, rectal hemorrhage, sialadenitis, stomatitis, tenesmus, tongue edema, ulcerative colitis[Ref]
Pancreatitis (including some fatalities) has been reported in patients using this drug, including those who developed hypertriglyceridemia.
Limit for high chemistry included amylase greater than 2 times the upper limit of normal (2 x ULN).[Ref]
Metabolic
Very common (10% or more): Increased cholesterol (up to 65.2%), increased triglycerides (up to 33.6%)
Common (1% to 10%): Increased fasting triglycerides, hypertriglyceridemia, increased uric acid, hypercholesterolemia, increased glucose, gout, dehydration, anorexia, increased alkaline phosphatase, decreased potassium, decreased calcium
Uncommon (0.1% to 1%): Diabetes mellitus, increased magnesium, increased LDH, increased chloride, increased potassium, decreased sodium, decreased chloride, decreased magnesium
Rare (0.01% to 0.1%): Hyperglycemia
Frequency not reported: Alcohol intolerance, avitaminosis, enzymatic abnormality, xanthomatosis, redistribution/accumulation of body fat
Antiretroviral therapy:
-Frequency not reported: Redistribution/accumulation of body fat (including central obesity, dorsocervical fat enlargement, peripheral wasting, facial wasting, breast enlargement, "cushingoid appearance"), increased blood lipid levels, increased glucose levels
Protease inhibitor therapy:
-Postmarketing reports: New onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, hyperglycemia, diabetic ketoacidosis[Ref]
Limits for high chemistry included cholesterol greater than 240 mg/dL, triglycerides greater than 800 mg/dL, triglycerides greater than 1500 mg/dL (greater than 16.9 mmol/L), fasting triglycerides greater than 1500 mg/dL (greater than 16.9 mmol/L), uric acid greater than 12 mg/dL (greater than 0.7 mmol/L), glucose greater than 13.8 mmol/L, alkaline phosphatase greater than 550 units/L, LDH greater than 1170 units/L, chloride greater than 122 mmol/L, and potassium greater than 6 mmol/L. Limits for low chemistry included potassium 3 mmol/L, calcium less than 3.45 mmol/L, chloride less than 84 mmol/L, magnesium less than 1 mmol/L, and sodium less than 123 mmol/L.
Increases of 30% to 40% from baseline have been reported for cholesterol levels and 200% to 300% for triglycerides.
Dehydration (usually associated with GI symptoms, and sometimes resulting in hypotension, syncope, or renal insufficiency) has been reported (including during postmarketing experience); orthostatic hypotension, syncope, and renal insufficiency have also been reported without known dehydration.
Hyperglycemia has also been reported during postmarketing experience in patients with and without known history of diabetes.
New onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, and hyperglycemia have been reported in HIV-infected patients receiving protease inhibitors; in some cases, diabetic ketoacidosis occurred. No causal relationship has been established.[Ref]
Nervous system
Very common (10% or more): Paresthesia (including oral and peripheral paresthesia; up to 50.7%), dysgeusia (16.2%), dizziness (up to 15.6%), taste perversion (up to 15.5%), peripheral neuropathy (10.1%), headache
Common (1% to 10%): Syncope, seizure, somnolence
Frequency not reported: Abnormal gait, amnesia, aphasia, ataxia, coma, convulsion, dementia, grand mal convulsion, hearing impairment, hyperesthesia, hyperkinesia, hypoesthesia, incoordination, migraine, neuralgia, neuropathy, paralysis, peripheral neuropathic pain, peripheral sensory neuropathy, sleep disorder, speech disorder, stupor, subdural hematoma, tinnitus, tremor, vertigo, vestibular disorder, cerebral ischemia, cerebral venous thrombosis, taste loss
Postmarketing reports: Neurologic events[Ref]
Syncope and seizure have also been reported during postmarketing experience.
Cardiac and neurologic events have been reported during postmarketing experience when this drug was used with disopyramide, mexiletine, nefazodone, fluoxetine, and beta blockers. Possible drug interaction could not be excluded.[Ref]
Other
Limit for low chemistry included albumin less than 20 g/L.
Acute ergot toxicity has been reported when this drug was used with ergotamine or dihydroergotamine.[Ref]
Very common (10% or more): Fatigue (including asthenia; 46.2%), asthenia (up to 14.2%), flushing/feeling hot (13.2%)
Common (1% to 10%): Edema, peripheral edema, peripheral coldness, fever, weight loss, malaise
Uncommon (0.1% to 1%): Decreased albumin
Frequency not reported: Breast pain, enlarged abdomen, accidental injury, cachexia, chest pain, chills, facial edema, facial pain, influenza syndrome, hypothermia, neck pain, neck rigidity, pain (unspecified), pelvic pain, substernal chest pain, ear pain, increased cerumen, parosmia, thirst
Postmarketing reports: Acute ergot toxicity (characterized by vasospasm, ischemia of extremities and other tissues [including the central nervous system])
Antiretroviral therapy:
-Frequency not reported: Increased weight[Ref]
Hematologic
Very common (10% or more): Decreased WBCs (up to 36.9%), decreased RBCs (up to 18.6%), decreased hematocrit (up to 17.3%)
Common (1% to 10%): Decreased neutrophils, decreased hemoglobin, thrombocytopenia, increased eosinophils, increased neutrophils, increased WBCs
Uncommon (0.1% to 1%): Increased prothrombin time, decreased platelet count
Frequency not reported: Acute myeloblastic leukemia, anemia, ecchymosis, leukopenia, lymphadenopathy, lymphocytosis, myeloproliferative disorder
Protease inhibitor therapy:
-Frequency not reported: Increased bleeding (including spontaneous skin hematomas, hemarthrosis) in hemophiliacs[Ref]
Limits for low hematology included WBCs less than 2.5 x 10(9)/L, RBCs less than 3 x 10(12)/L, hematocrit less than 30% (less than 0.3), neutrophils up to 0.5 x 10(9)/L, hemoglobin less than 8 g/dL, and platelet count less than 2 x 10(9)/L. Limits for high hematology included eosinophils greater than 1 x 10(9)/L, neutrophils greater than 20 x 10(9)/L, WBCs greater than 25 x 10(9)/L, and prothrombin time greater than 1.5 x ULN.
Increased bleeding (including spontaneous skin hematomas and hemarthrosis) in patients with hemophilia type A or B treated has been associated with protease inhibitors. In many of the reported cases, treatment with protease inhibitors was continued or restarted and some patients required additional factor VIII. A causal relationship between protease inhibitor therapy and these episodes has not been established.[Ref]
Dermatologic
Very common (10% or more): Rash (including erythematous rash, maculopapular rash; up to 27.1%), pruritus (up to 12.2%)
Common (1% to 10%): Acne, acquired lipodystrophy, sweating
Rare (0.01% to 0.1%): Stevens-Johnson syndrome, toxic epidermal necrolysis
Frequency not reported: Contact dermatitis, dry skin, eczema, erythema multiforme, exfoliative dermatitis, folliculitis, fungal dermatitis, furunculosis, maculopapular rash, molluscum contagiosum, onychomycosis, photosensitivity reaction, psoriasis, pustular rash, seborrhea, skin discoloration, skin disorder, skin hypertrophy, skin melanoma, urticaria, vesiculobullous rash, alopecia[Ref]
Toxic epidermal necrolysis has also been reported during postmarketing experience.
Alopecia has been reported in patients using indinavir or atazanavir plus this drug.[Ref]
Respiratory
Very common (10% or more): Coughing (21.7%), oropharyngeal pain (15.9%), pharyngitis
Frequency not reported: Asthma, bronchitis, increased cough, dyspnea, epistaxis, hiccup, hypoventilation, interstitial pneumonia, larynx edema, lung disorder, rhinitis, sinusitis[Ref]
Hepatic
Very common (10% or more): Increased GGT (up to 19.6%)
Common (1% to 10%): Increased AST, increased ALT, hepatitis (including increased AST, ALT, GGT), increased blood bilirubin (including jaundice), increased total bilirubin
Frequency not reported: Exacerbation of chronic liver disease, cholangitis, cholestatic jaundice, hepatic coma, hepatomegaly, hepatosplenomegaly, liver damage, liver function tests abnormal, hepatic transaminase elevations exceeding 5 x ULN, clinical hepatitis, jaundice
Postmarketing reports: Hepatic dysfunction (including some fatalities)[Ref]
Limits for high chemistry included GGT greater than 300 international units/L, AST greater than 180 international units/L, ALT greater than 215 international units/L, and total bilirubin greater than 61 mcmol/L.
Hepatic dysfunction (including some fatalities) has been reported, generally in patients taking multiple concurrent medications and/or with advanced AIDS.[Ref]
Musculoskeletal
Limit for high chemistry included CPK greater than 1000 international units/L.
Osteonecrosis has been reported, particularly in patients with advanced HIV disease, long-term combination antiretroviral therapy, or other risk factors (including corticosteroid use, alcohol use, severe immunosuppression, higher body mass index).[Ref]
Very common (10% or more): Arthralgia and back pain (18.6%), increased creatine phosphokinase (CPK; up to 12.1%)
Common (1% to 10%): Myalgia, myopathy/increased CPK, myositis, rhabdomyolysis
Frequency not reported: Arthritis, arthrosis, bone disorder, bone pain, extraocular palsy, joint disorder, leg cramps, muscle cramps, muscle weakness, twitching, osteonecrosis[Ref]
Hypersensitivity
Common (1% to 10%): Hypersensitivity (including urticaria, face edema)
Rare (0.01% to 0.1%): Anaphylaxis
Frequency not reported: Allergic reactions (including urticaria, mild skin eruptions, bronchospasm, angioedema)[Ref]
Ocular
Common (1% to 10%): Blurred vision
Frequency not reported: Abnormal electrooculogram, abnormal electroretinogram, abnormal vision, amblyopia/blurred vision, blepharitis, conjunctivitis, diplopia, eye disorder, eye pain, iritis, photophobia, uveitis, visual field defect, vitreous disorder[Ref]
Genitourinary
Common (1% to 10%): Increased urination, menorrhagia
Frequency not reported: Albuminuria, cystitis, dysuria, glycosuria, hematuria, impotence, nocturia, penis disorder, polyuria, urethritis, urinary frequency, urinary retention, urinary tract infection, vaginitis[Ref]
Menorrhagia has also been reported during postmarketing experience.[Ref]
Cardiovascular
Myocardial infarction has also been reported during postmarketing experience.
Cardiac and neurologic events have been reported during postmarketing experience when this drug was used with disopyramide, mexiletine, nefazodone, fluoxetine, and beta blockers. Possible drug interaction could not be excluded.[Ref]
Common (1% to 10%): Hypertension, hypotension (including orthostatic hypotension), vasodilation
Uncommon (0.1% to 1%): Myocardial infarction
Frequency not reported: PR interval prolonged, cardiovascular disorder, palpitation, peripheral vascular disorder, phlebitis, postural hypotension, tachycardia, vasospasm, hemorrhage
Postmarketing reports: Orthostatic hypotension, first-degree atrioventricular (AV) block, second-degree AV block, third-degree AV block, right bundle branch block, cardiac events[Ref]
Psychiatric
Common (1% to 10%): Confusion, disturbance in attention, insomnia, anxiety, abnormal thinking
Frequency not reported: Abnormal dreams, depression, depersonalization, emotional lability, euphoria, agitation, hallucinations, decreased libido, manic reaction, nervousness, personality disorder
Renal
Limit for high chemistry included creatinine greater than 0.3 mmol/L.
Renal insufficiency was reported in 3 AIDS patients receiving this drug. All cases occurred within 10 to 15 days after starting this drug and all were reversible upon discontinuation.[Ref]
Common (1% to 10%): Renal impairment (e.g., oliguria, elevated creatinine)
Uncommon (0.1% to 1%): Acute renal failure, increased creatinine
Frequency not reported: Renal calculus, renal failure, abnormal kidney function, kidney pain, pyelonephritis, increased BUN
Postmarketing reports: Renal insufficiency, nephrolithiasis[Ref]
Immunologic
Frequency not reported: Immune reconstitution syndrome, autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome, autoimmune hepatitis)
Endocrine
Common (1% to 10%): Decreased free and total thyroxin
Frequency not reported: Adrenal cortex insufficiency, hormone level altered
Postmarketing reports: Cushing's syndrome, adrenal suppression[Ref]
Cushing's syndrome and adrenal suppression have been reported when this drug was used with fluticasone or budesonide.[Ref]
More about ritonavir
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (3)
- Drug images
- Dosage information
- During pregnancy
- Drug class: antiviral boosters
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Markowitz M, Saag M, Powderly WG, Hurley AM, Hsu A, Valdes JM, Henry D, Sattler F, La Marca A, Leonard JM, et al. A preliminary study of ritonavir, an inhibitor of HIV-1 protease, to treat HIV-1 infection. N Engl J Med. 1995;333:1534-9.
2. Product Information. Norvir (ritonavir). Abbott Pharmaceutical. 2001;PROD.
3. Carr A. HIV protease inhibitor-related lipodystrophy syndrome. Clin Infect Dis. 2000;30:s135-42.
4. Michelet C, Ruffault A, Sebille V, et al. Ritonavir-saquinavir dual protease inhibitor compared to ritonavir alone in human immunodeficiency virus-infected patients. Antimicrob Agents Chemother. 2001;45:3393-402.
5. Aarnoutse RE, Droste JA, Van Oosterhout JJ, et al. Pharmacokinetics, food intake requirements and tolerability of once-daily combinations of nelfinavir and low-dose ritonavir in healthy volunteers. Br J Clin Pharmacol. 2003;55:115-125.
6. Cerner Multum, Inc. UK Summary of Product Characteristics.
7. Brennan-Benson P, Pakianathan M, Rice P, et al. Enfurvitide prevents vertical transmission of multidrug-resistant HIV-1 in pregnancy but does not cross the placenta. AIDS. 2006;20:297-9.
8. Warnke D, Barreto J, Temesgen Z. Antiretroviral drugs. J Clin Pharmacol. 2007;47:1570-9.
9. Cerner Multum, Inc. Australian Product Information.
10. Merry C, Barry M, Gibbons S, Mulcahy F, Back D. Improved tolerability of ritonavir derived from pharmacokinetic principles. Br J Clin Pharmacol. 1996;42:787.
11. von Hentig N, Muller A, Rottmann C, et al. Pharmacokinetics of saquinavir, atazanavir and ritonavir in a boosted double-protease inhibitor twice-daily regimen. Antimicrob Agents Chemother. 2007;51:1431-9.
12. Tsiodras S, Mantzoros C, Hammer S, Samore M. Effects of protease inhibitors on hyperglycemia, hyperlipidemia, and lipodystrophy - A 5-year cohort study. Arch Intern Med. 2000;160:2050-6.
13. Dube M, Fenton M. Lipid abnormalities. Clin Infect Dis. 2003;36(Suppl 2):S79-83.
14. Fantoni M, Del Borgo C, Autore C. Evaluation and management of metabolic and coagulative disorders in HIV-infected patients receiving highly active antiretroviral therapy. AIDS. 2003;17 Suppl 1:S162-9.
15. Fontas E, Van Leth F, Sabin CA, et al. Lipid Profiles in HIV-Infected Patients Receiving Combination Antiretroviral Therapy: Are Different Antiretroviral Drugs Associated with Different Lipid Profiles? J Infect Dis. 2004;189:1056-74.
16. Brown CA, Lesher JL Jr, Peterson CM. Tuberous and tendinous xanthomata secondary to ritonavir-associated hyperlipidemia. J Am Acad Dermatol. 2005;52(5 Suppl 1):S86-9.
17. Bergersen BM. Cardiovascular Risk in Patients with HIV Infection : Impact of Antiretroviral Therapy. Drugs. 2006;66:1971-87.
18. Lee GA, Rao M, Mulligan K, et al. Effects of ritonavir and amprenavir on insulin sensitivity in healthy volunteers. AIDS. 2007;21:2183-90.
19. Manfredi R, Calza L, Chiodo F. Gynecomastia associated with highly antiretroviral therapy. Ann Pharmacother. 2001;35:438-9.
20. Ginarte M, Losada E, Prieto A, Lorenzo-Zuniga V, Toribio J. Generalized hair loss induced by indinavir plus ritonavir therapy. AIDS. 2002;16:1695-6.
21. Torres HA, Barnett BJ, Arduino RC. Alopecia associated with ritonavir-boosted atazanavir therapy. AIDS. 2007;21:1391-1392.
22. Lee D, Benson CA, Lewis CE, Grunfeld C, Scherzer R. Prevalence and factors associated with dry skin in HIV infection: the FRAM study. AIDS. 2007;21:2051-2057.
23. Soriano V, Puoti M, Sulkowski M, et al. Care of patients coinfected with HIV and hepatitis C virus: 2007 updated recommendations from the HCV-HIV International Panel. AIDS. 2007;21:1073-89.
24. Schrooten W, Colebunders R, Youle M, et al. Sexual dysfunction associated with protease inhibitor containing highly active antiretroviral treatment. AIDS. 2001;15:1019-23.
25. Duong M, Sgro C, Grappin M, Biron F, Boibieux A. Renal failure after treatment with ritonavir. Lancet. 1996;348:693-4.
26. Chugh S, Bird R, Alexander EA. Ritonavir and renal failure. N Engl J Med. 1997;336:138.
27. Izzedine H, Launay-Vacher V, Deray G. Antiviral drug-induced nephrotoxicity. Am J Kidney Dis. 2005;45:804-17.
28. Roling J, Schmid H, Fischereder M, Draenert R, Goebel FD. HIV-Associated Renal Diseases and Highly Active Antiretroviral Therapy-Induced Nephropathy. Clin Infect Dis. 2006;42:1488-95.
29. Barbour TD, Furlong TJ, Finlayson RJ. Efavirenz-associated podocyte damage. AIDS. 2007;21:257-258.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.